Dr. Richard S. Roth is an Infectious Disease Specialist in Savannah, Georgia. He graduated with honors from Tulane University School Of Medicine in 1988. He has over 30 years of diverse experience especially in infectious diseases. Dr. Roth is Board Certified in Infectious Disease Internal Medicine. He is a Fellow in the Civil Aviation Medical Association and he is a consultant to FAA, NTSB and Pilot Medical Solutions – LeftSeat.com. Dr. Roth is also an instructor for Flight Safety International. Information and medical perspective concerning COVID-19 changes constantly. It is not possible to keep pace with this rapidly changing field of information. Consult directly with your physician or Dr. Roth for current guidance.
Types of Vaccines:
Inactivated or weakened virus vaccines, which use a form of the virus that has been inactivated or weakened so it does not cause disease, but still generates an immune response.
Protein-based vaccines, which use harmless fragments of proteins or protein shells that mimic the COVID-19 virus to safely generate an immune response.
Viral vector vaccines, which use a virus that has been genetically engineered so that it cannot cause disease but produces coronavirus proteins to safely generate an immune response.
RNA and DNA vaccines, a cutting-edge approach that uses genetically engineered RNA or DNA to generate a protein that itself safely prompts an immune response.
How do the Pfizer and Moderna mRNA vaccines work?
The vaccines contain synthetic mRNA, which is genetic information used to make the SARS-CoV-2 spike protein. The spike protein is the part of the virus that attaches to human cells. The spike protein alone cannot cause COVID-19. Once the spike protein is created, it causes the immune system to make antibodies against the virus. These antibodies can then provide protection if a person comes into contact with the virus. The mRNA vaccines are non-infectious and do not enter the human cell nucleus, so they cannot be inserted into human DNA. Additionally, mRNA is rapidly broken down, and this theoretically reduces chances for long-term side effects. The mRNA vaccines do not have the ability to cause cancer.
FDA and FAA Approvals:
Following the Emergency Use Authorization from the U.S. Food and Drug Administration (FDA) for Pfizer’s and Modena’s COVID-19 vaccine, the FAA has determined that pilots may receive the vaccine under the conditions of their FAA-issued airman medical certification. FAA Air Traffic Controllers, who are subject to FAA medical clearance, may also receive the vaccine.
To maintain the highest level of safety in the National Airspace System, the agency will require pilots with medical certifications or air traffic controllers with medical clearances to observe a period of 48 hours following the administration of each dose of this vaccine before conducting safety-sensitive aviation duties, such as flying or controlling air traffic.
Because the Moderna vaccine requires two doses, 28 days apart for maximum effectiveness, the waiting period applies after each dose. The Pfizer vaccine, which was approved last week, requires two doses 21 days apart, but the waiting period after each dose applied to both brands.
The FAA anticipates taking no additional measures to ensure safety after the initial window for side effects closes. However, the agency’s medical professionals will continuously monitor the initial distribution of the novel vaccine and documented clinical results and will adjust these recommendations as needed.
The FAA encourages Americans to receive COVID-19 vaccinations as authorized by FDA. This policy announcement pertains to a specialized group of FAA-certificated persons who perform safety-sensitive aviation duties.
Side effects: (NOT defined as Adverse Events):
The most common side effects of the vaccine are like some routine vaccines, including a sore arm, tiredness, headache, and muscle pain.
Why are there still outbreaks of vaccine-preventable diseases?
Measles was declared eliminated in 2000. Yet in 2019, there were 1,282 cases reported in the U.S. Outbreaks of vaccine-preventable diseases still occur when too few individuals in a population are vaccinated. Outbreaks often begin with an imported case (someone who was travelling outside the U.S.) or person encountering an unvaccinated individual or people. These infected people then expose unprotected people to the disease. There are a number of reasons why people are unprotected: some protection from vaccines “wanes” or “fades” after a period of time. Some people don’t receive all of the shots that they should to be completely protected. For example you need two measles, mumps, and rubella (MMR) injections to be adequately protected. Some people may only receive one and mistakenly believe they are protected. Some people may object because of religious reasons, and others are fearful of potential side effects or are skeptical about the benefits of vaccines.
False positive HIV tests after Covid19 vaccination:
British and French pharmaceutical giants GlaxoSmithKline and Sanofi Pasteur said the release of their vaccine would be pushed to late next year, while one of Australia’s four vaccine candidates was axed after trial participants returned false positive test results for HIV. The announcements could present a potential setback in the global effort to gain control of the pandemic, given that experts believe that multiple vaccine options will be required to do so. This DID NOT occur in the Moderna nor the Pfizer trials.
What is contained in a dose of the Pfizer or Moderna mRNA vaccines:
The vaccines contain only the mRNA molecules which codes for the spike protein that our body then develops the effective antibody against. This antibody product our body makes (called a titer) is made significantly better by the vaccine than if we were to be been infected by the real Covid19 virus itself.
The mRNA molecule NEVER enters our nucleus of our cells, NEVER incorporates in our native DNA and quickly is destroyed by our own defenses post injection yet is active long enough to enable the spike protein of Covid19 to be produced that our own body then develops the protective antibodies against with give us subsequently the umbrella of immunity ie: protection.
What are the vaccine ingredients?
Pfizer-BioNTech – mRNA (active ingredient)
Lipids (0.43 mg (4-hydroxybutyl)azanediyl)bis(hexane-6,1-diyl)bis(2-hexyldecanoate), 0.05 mg 2[(polyethylene glycol)-2000]-N,N-ditetradecylacetamide, 0.09 mg 1,2-distearoyl-sn-glycero-3- phosphocholine, and 0.2 mg cholesterol)
Potassium chloride
Monobasic potassium phosphate
Sodium chloride
Dibasic sodium phosphate dihydrate
Sucrose
Moderna – mRNA (active ingredient)
Lipids (SM-102, 1,2-dimyristoyl-rac-glycero3-methoxypolyethylene glycol-2000 [PEG2000-DMG], cholesterol, and 1,2-distearoyl-snglycero-3-phosphocholine [DSPC])
Tromethamine
Tromethamine hydrochloride
Acetic acid
Sodium acetate
Sucrose
In the vial of the mRNA vaccines are lipids (cholesterol) as a carrying agent and salts for neutrality of the solution. There are NO PRESERVATIVES, NO MECURY, NO THIMERSOL nor nano-surveillance chips in the product. The mRNA vaccines are not an extension of the unfortunate Tuskegee syphilis study uncovered and openly condemned by all decades ago.
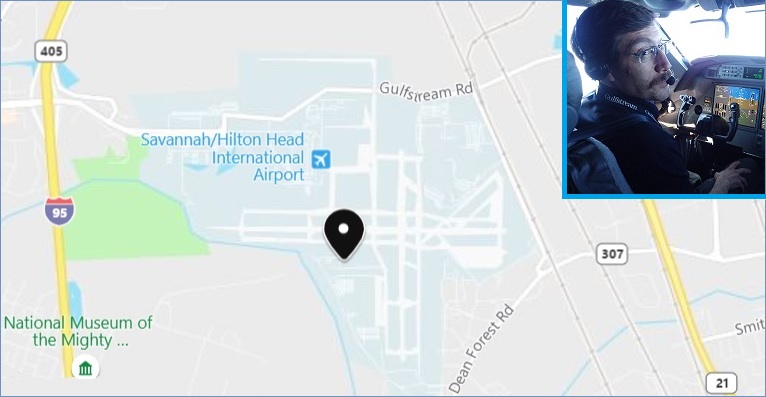
Richard S. Roth, MD
Roth Aviation Medical Services
100 Eddie Jungemann Drive
Savannah, Georgia 31408
PHONE: 912-964-7684 | SavannahAME.com